Bacterial antibiotic resistance is on the rise. This developing resilience in bacteria, to the very drugs we use to rorevent infection, will render our current antibiotics useless within the next few decades. Already it is estimated that 25,000 people die annually within Europe from antibiotic resistance.
What is more the pipeline for new antibiotics is drying up with only two new classes of antibiotics being brought to market since 1962, compared to more than 20 new classes of antibiotics marketed between 1940 and 1962.
This week a team led by Professor Kim Lewis from Northeastern University have published the discovery of a new antibiotic, teixobactin. Importantly in current tests this antibiotic seems itself resistant to the build-up of resistance in bacteria, which means that it may buy us more time in the fight against antibiotic resistance, whilst the bugs have to adapt and work out ways to get round our latest lines of attack.
Equally important in the identification of this compound is the new method, the iChip, which was used to isolate it. This method of studying environmentally diverse bacteria under laboratory conditions means that we can now analyse a wider range of bacteria than previously possible. This effectively increases the size of the pool we have in which to pan for new drugs, and with any luck may yield plenty more.
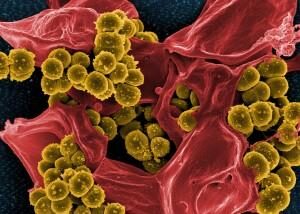
Methicillin-resistant Staphylococcus aureus
The World Health Organisation last year noted the need for new diagnostic advances to improve the speed of patient testing. Current tests take too long to run, with samples typically taking 16-20 hours to be processed by hospital labs. Consequently physicians often forego them and prescribe broad-spectrum antibiotics. Faster tests would lead to more targeted drug treatments helping to safeguard current medications.
A publication in Science Translational Medicine at the end of last year saw a possible victory in the fight against resistance. Engineering innovation allowed a team of researchers at Seoul National University to develop a test which can identify bacteria that will respond to antibiotics with a 3-4 hour turnaround. This is done by analysing how single bacterial cells change structurally in the presence of various antibiotics. The Korean team tested strains of Escherichia coli, Pseudomonas aeruginosa, Klebsiella pneumoniae, Staphylococcus aureus and Enterococcus spp. and were able to determine within a few hours which strains would respond to treatment. This could provide a possible game-changer for the over-prescription of antibiotics and help to protect the drugs we currently use.
Despite the possible advances and savings in unnecessary antibiotic prescriptions this technology could bring, we are unlikely to see its implementation in hospitals any time soon. This requires tools far beyond those found in a typical lab and would require significant financial investment, which is simply not available in many healthcare systems.
Another diagnostic test which could be implemented in the clinical setting to prevent the overuse of antibiotics is for procalcitonin. Procalcitonin is the precursor form of calcitonin and is produced by many different cell types, albeit at undetectable levels in healthy people. In the case of sepsis procalcitonin levels increase and are indicative for progression to severe sepsis and septic shock. Procalcitonin levels can therefore help to determine whether patients are suffering from bacterial or viral infections and guide treatment accordingly.
Tests for procalcitonin levels are beginning to be used in UK hospitals to assess whether incoming patients are at risk of sepsis and help to decide whether or not to treat with antibiotics. The implementation of procalcitonin testing in intensive care and emergency departments may help to identify patients who do not need antibiotics, and target antibiotic therapy more effectively. Without rapid clinical evidence of bacterial infection many clinicians prescribe antibiotics ‘just in case’. It is this ‘just in case’ syndrome that adds significantly to the over-prescription of antibiotics, particularly for cases of acute respiratory infection (for which the greatest tonnage of antibiotics are prescribed).
However, numerous studies have now shown that procalcitonin levels can be used to guide treatment of respiratory infection with antibiotics. When the initiation or discontinuation of antibiotic administration was based on procalcitonin levels in the blood no increases patient morbidity or mortality were shown, yet a reduction was observed across all studies in the amount of antibiotics used. Similar results have been seen for procalcitonin testing in patients of chronic obstructive pulmonary disease. When procalcitonin levels were taken into account in making treatment decisions antibiotics were better directed to those who needed them, with less waste to those who did not.
A comparison of the cost-effectiveness of the use of procalcitonin testing in guiding antibiotic administration in cases of respiratory infection in adults show conflicting results. Some studies have demonstrated that the adoption of procalcitonin protocols do cost more than usual care. However, studies commissioned by NICE show a reduction in overall costs with the implementation of procalcitonin testing in clinics. Yet the societal costs of increasing antibiotic resistance and requirements for antimicrobial treatments may ultimately make procalcitonin testing a cost we must meet.
See our Affimer product catalogue.